This article was last updated on November 25, 2025.
You already feel the squeeze: every new application drops a 100-page PDF on your desk and the clock starts ticking. Manual record review consumes huge blocks of staff time and forces claims and underwriting decisions to wait in line. Paper-heavy claims workflows linger for weeks before payment moves forward.
Those hours spent manually processing documents represent your scaling constraint. While skilled processors handle perhaps 15 records per shift, AI agents process hundreds automatically, feeding structured, validated data directly into your underwriting, claims, and policy systems while maintaining compliance requirements.
This shifts your team from constant backlog firefighting to exception-based operations that scale as application numbers increase.
In this article, we'll explore how AI agents process medical records automatically, examine extraction capabilities across key insurance workflows, and provide a practical implementation approach.
How AI Agents Process Medical Records Automatically
Picture the stack of PDFs, faxes, and handwritten notes your team opens every morning. An intelligent agent turns that pile into structured, validated data before you finish your first coffee.
The workflow appears simple to watch but operates with remarkable complexity behind the scenes: documents flow into an intake queue, get classified by type, convert to text, undergo parsing for clinical meaning, validation against business rules, and finally push to your underwriting, claims, or policy platform.
Three core technologies make this end-to-end automation possible, each handling a critical part of the document processing pipeline:
Advanced Optical Character Recognition (OCR)
OCR converts low-resolution scans, fax images, and even messy handwriting into clean text. AI agents use deep-learning OCR paired with image enhancement to prevent poor lighting or tilted pages from derailing extraction.
Your operations deal with every document format imaginable: handwritten physician notes, consent forms, faxed reports, and low-resolution scans.
Modern agents clean, deskew, and digitize these automatically. Multi-page medical histories are stitched together to maintain context across sections, while structured tables like lab results are parsed alongside unstructured physician narratives.
Natural Language Processing (NLP)
NLP handles the clinical language itself, with named-entity recognition flagging diagnoses, drugs, and procedures, while relation extraction links medications to dosages or lab values to test dates. Once text is available, agents extract the specific fields that drive insurance decisions.
ICD-10 and CPT codes flow out with their corresponding procedure descriptions, medication lists emerge with dosing schedules and treatment histories, and lab values get captured alongside reference ranges and test dates. Provider identifiers, facility names, and encounter timestamps round out the structured data your systems need for processing.
Large Language Models (LLMs)
LLMs supply context by reading the entire record rather than a single page, reconciling conflicting entries and inferring missing details. These models also power the validation process that keeps data trustworthy.
AI systems assign confidence scores and route low-certainty fields to human reviewers, providing a human-in-the-loop safeguard for critical data. Protected health information stays encrypted in transit and at rest, with role-based access controls and comprehensive audit logs meeting HIPAA compliance requirements.
The final step transforms your operations entirely. Agents map outputs to standardized vocabularies like ICD-10, LOINC, and SNOMED, then hand off data to your policy admin system, claims engine, or data warehouse.
AI agents don't just automate templated processes—they learn from each correction to handle new document types without requiring re-coding. Your team shifts from spending hours extracting data to minutes reviewing exceptions, while structured, compliant medical data flows directly where your downstream workflows need it.
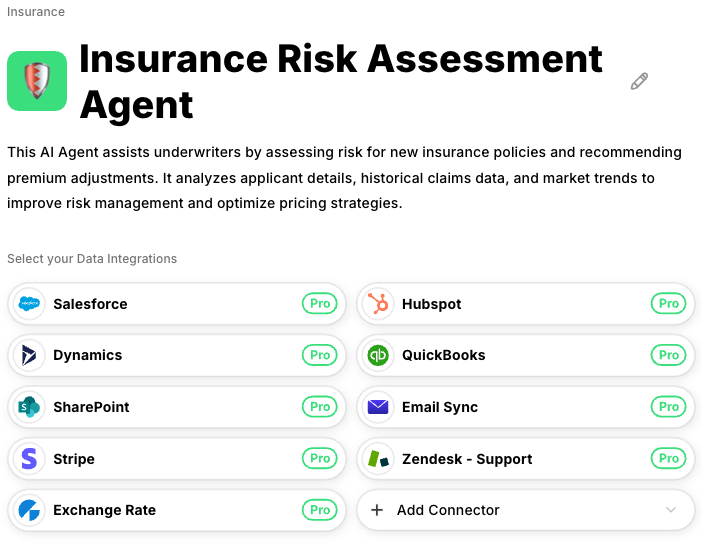
Datagrid's AI agents handle this entire pipeline automatically, connecting to policy administration systems, claims platforms, and underwriting tools through unified software. This eliminates the custom integration work typically required for each new document type or data source.
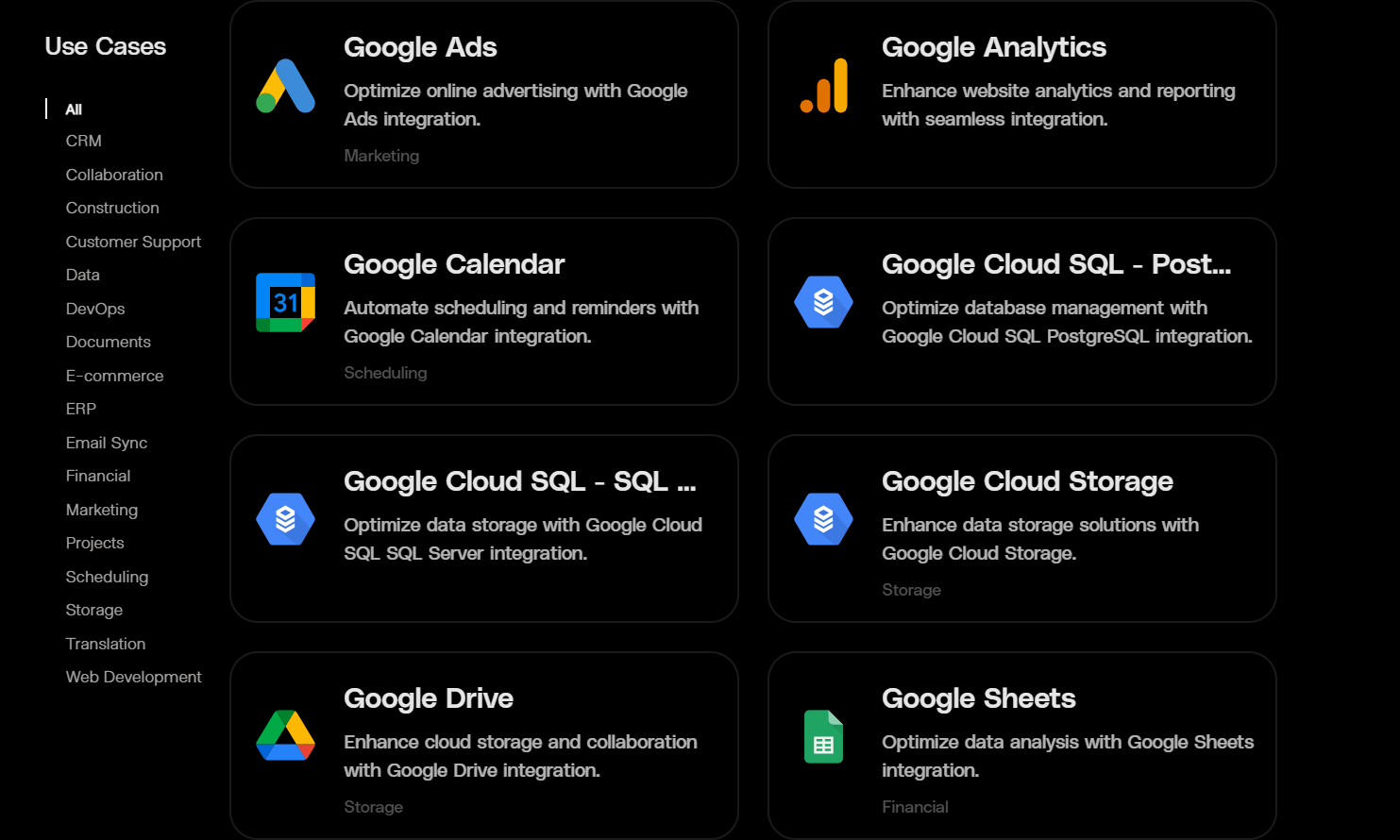
3 Insurance Workflows Where AI Agents Can Automate Medical Record Extraction
Automated extraction only matters when it meets your daily deadlines. These intelligent systems use the same core technologies—OCR for legibility, NLP for clinical context, and language models for reasoning—across three critical workflows: underwriting, claims, and policy administration.
Instead of forcing you to redesign systems, modern AI solutions provide a single pipeline that processes handwritten forms, faxed PDFs, and multi-page clinical narratives. The system delivers structured, queryable data directly to your existing platforms.
1. Underwriting Applications
New applications arrive with Attending Physician Statements that can stretch past 100 pages. Each document contains diagnoses, medications, and treatment histories you need before making risk decisions.
Intelligent agents classify document types and extract every ICD-10 code, procedure, and medication in seconds. AI extraction can export JSON that your underwriting system treats like native data, while advanced OCR prevents physician scrawl from creating delays.
Underwriting teams can trust this technology to handle routine files and surface only edge cases for expert review. Instead of multiday queues, you get same-day medical data and can issue decisions while applicant attention is fresh. Teams that once processed a few dozen files daily now handle triple or quadruple that volume because software works in parallel instead of sequentially.
2. Claims Processing
Claims adjudication stalls because someone has to align CPT codes, treatment dates, and provider details scattered across bills, operative notes, and discharge summaries. Intelligent extraction changes this completely.
AI agents pull diagnosis and procedure codes directly from scanned paperwork, even when each hospital uses different layouts, then validate data against internal business rules before releasing it downstream.
The system adds safety by cross-checking narrative descriptions for inconsistencies, duplicates, or fraud patterns. Your adjusters open claim files to find every clinical field pre-populated and reconciled. What was a three-to-five-day bottleneck becomes a matter of hours, letting teams focus on negotiation and customer communication rather than data entry.
Pattern-matching models flag ambiguous fields and pull ICD-10 codes with consistency no human team can replicate at scale. This leads to fewer mistakes, fewer denials, faster adjudication, and cleaner audit trails.
3. Policy Administration
Annual medical updates quietly balloon workload as active policies trigger document reviews at renewal. Modern AI agent systems neutralize that spike. The same extraction pipeline that handled underwriting now monitors for new physician notes, lab results, or medication changes, pulling only relevant deltas into the policy system.
These AI solutions learn to recognize evolving document formats automatically, eliminating retraining for every new clinic. Historical snapshots remain visible, letting agents flag meaningful shifts—new chronic diagnoses or discontinued medications—that might alter premiums or exclusions.
You process higher volumes without seasonal staffing surges and keep renewals on schedule instead of reacting to backlog crises. This automation can reduce documentation labor by nearly two-thirds in most pilots, freeing up staff time for higher-value analysis, customer outreach, and complex exception handling.
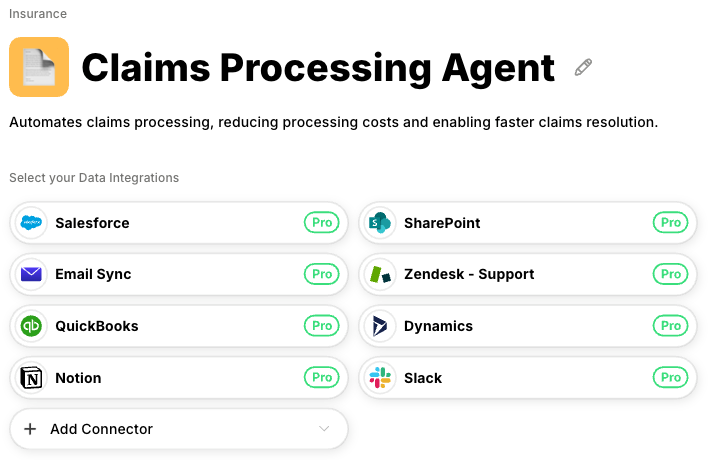
How Datagrid Handles Multi-Workflow Medical Record Extraction
Datagrid deploys specialized AI agents trained for insurance document processing across underwriting, claims, and policy administration workflows. These agents access medical records from multiple sources while maintaining HIPAA compliance and enterprise security standards insurance operations require.
Implementation Approach
The fastest way to eliminate your manual medical record backlog starts with a simple principle: begin small, measure everything, and expand only when the numbers prove it works.
Begin with a narrow pilot targeting high-volume document types. Scanned documents like lab reports or standard Attending Physician Statements work well because their layouts are predictable. AI agents can process these documents immediately, so you spend your first weeks configuring business rules rather than training models from scratch.
Measuring success requires clear metrics:
- Time how long experienced staff need to extract each field
- Track error rates across different document types
- Log system hand-offs and integration points
- Compare each agent output iteration against your baseline
Setting up validation protocols that work automatically ensures quality control. Modern systems assign confidence scores to every extracted field, routing low-confidence items to human reviewers without manual sorting.
Datagrid's agent platform includes validation protocols and confidence scoring by default, with built-in exception routing that lets operations managers prove accuracy improvements during pilot programs. This allows you to demonstrate ROI with real extraction comparisons before expanding to production workflows.
AI agents surface these scores in real time, letting you verify accuracy without reviewing entire records.
Between lower labor costs, faster premium recognition, and reduced error remediation, insurers using AI automation commonly achieve substantial efficiency gains. Manual review stretches processing time to a full workweek while records wait in queue; automation cuts that to same-day turnaround by extracting data the moment a PDF or fax arrives.
This rapid payback means your seasoned analysts finally focus on tough edge cases while intelligent agents handle the repetitive work—letting your operation scale with demand instead of headcount.
Eliminate Medical Record Processing Bottlenecks with Datagrid
Datagrid's AI agents automate medical record extraction across your insurance operations:
- Multi-format document processing: AI agents handle handwritten physician notes, faxed records, scanned PDFs, and multi-page medical histories automatically, extracting diagnosis codes, treatment histories, and medication lists without manual data entry.
- Cross-workflow automation: The same agent platform processes medical records for underwriting applications, claims adjudication, and policy administration renewals, eliminating the need to build separate extraction systems for each workflow.
- Enterprise security and compliance: HIPAA-compliant processing includes encrypted data handling, role-based access controls, and comprehensive audit trails that meet regulatory requirements without custom security configuration.
- Validation and exception routing: Confidence scoring flags low-certainty extractions for human review automatically, letting your experienced staff focus on complex cases while agents handle routine document processing.
- Seamless system integration: Agents connect to policy administration platforms, claims systems, and underwriting tools through unified APIs, pushing structured medical data directly where your workflows need it without point-to-point integration work.
Get started with Datagrid to automate medical record extraction across your insurance operations.