This article was last updated on December 9, 2025
Manual data extraction from claim forms still swallows most of a claims professional's day. When 46% of health insurance claim denials stem from missing or incorrect information, the problem isn't your team's expertise, it's the hours spent re-typing names, codes, and policy numbers into core systems.
During storms or open-enrollment peaks, simple claims that should close in days can drag on for weeks, leaving payments and policyholders in limbo. Backlogs balloon, adjusters chase missing data, and customers call for updates that don't exist.
This guide covers today's manual workflow reality, what automated processing delivers, and seven practical implementation steps that transform operations.
How Claims Forms Are Processed Today
Claims arrive through dozens of channels like portal uploads, email attachments, mobile photos, and even fax machines. Each submission enters a manual pipeline where staff re-key information into core systems, chase missing documents, validate coverage against policy records, and route files through multi-level approval before releasing payment.
Every handoff creates failure points. Processing errors hit nearly one in five claims, triggering denials, resubmissions, and frustrated customers. Simple submissions stretch from days into weeks as adjusters wait for corrected information.
Volume makes everything worse. Your team jumps between screens to capture data, applies inconsistent validation rules, and reworks files when information doesn't reconcile. Each manually processed medical claim can cost $12–$19, draining millions annually from health providers.
Peak periods expose the bottlenecks. Document retrieval consumes significant portions of a home-claims handler's day, and many struggle with manual document review. Without real-time visibility into service commitments, you're fighting backlogs instead of resolving claims.
What Automated Claims Forms Processing Looks Like
Claims adjusters spend their time moving data between systems instead of evaluating claims. Every submission requires manual data entry across multiple screens, validation against policy records, and routing decisions that create bottlenecks during peak periods.
Automated processing eliminates this data transfer burden through three core capabilities:
Intelligent Document Capture and Extraction
AI agents capture information from any format (PDFs, photos, portal submissions) and extract key fields with contextual understanding.
Unlike legacy scanning systems that create static digital files, intelligent document processing understands relationships between data points.
When a diagnosis code appears next to a service date, the system correctly links the code to the treatment, not the admission.
This contextual awareness drives high accuracy rates on medical and billing forms, eliminating the manual errors that plague traditional workflows. Adjusters focus on complex evaluations, not keystrokes.
Automated Validation and Decision Processing
Decision engines validate against policy rules and compare extracted data against coverage limits, deductibles, and regulatory requirements without manual cross-checking.
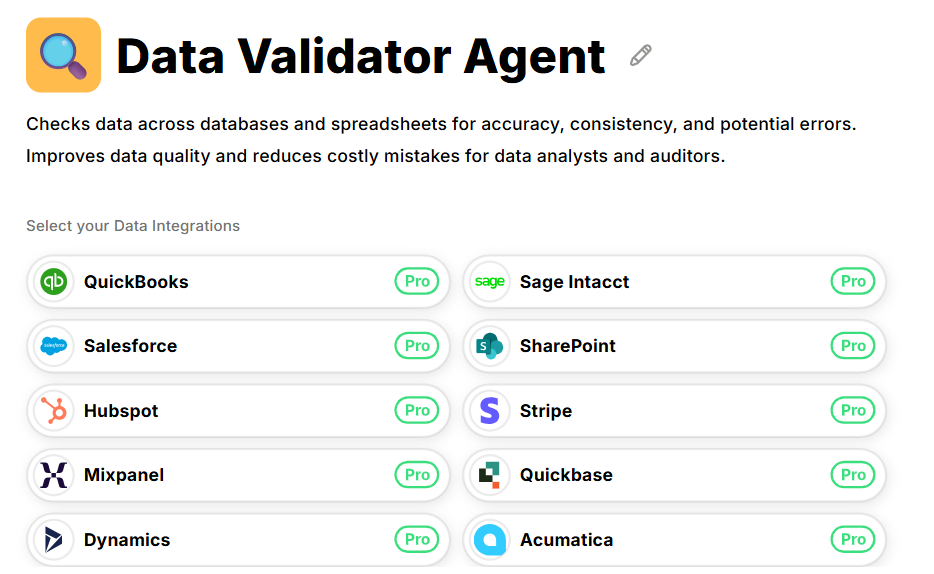
Coverage status, policy limits, prior claim history, and fraud markers are all checked in milliseconds by Datagrid's Data Validator Agent.
This automation avoids the manual costs baked into every medical claim that relies on swivel-chair lookups between systems.
End-to-End Workflow Orchestration
Workflow automation updates core systems, triggers correspondence, and routes submissions to the right destination while maintaining complete audit trails throughout.
Claims flow through the appropriate processing lane automatically, from instant payment for straightforward submissions to specialist review for complex losses.
Results show up immediately on operational metrics. Insurers using AI-driven intake cut manual document handling significantly and increase capacity during surge periods.
Auto carriers applying computer vision to damage photos settle straightforward submissions in minutes instead of days, freeing adjusters for complex losses.
Speed with accuracy reduces rework, lowers cost per claim, and delivers the fast settlement experience policyholders expect.
How to Implement Automated Claims Forms Processing
Rolling out automation works best as a phased journey rather than wholesale replacement. Start small and expand in steady increments to protect daily operations while capturing benefits.
Step 1: Map Your Claims Forms and Intake Channels
Begin with a complete inventory of your current operations. List every claim type (auto glass, outpatient health, property damage), then document how each arrives (agency portals, email attachments, mobile uploads, fax).
Focus on high-volume submissions and documents that drive the most rework. A whiteboard session with front-line adjusters typically surfaces the dozen forms that should anchor your first rollout.
Step 2: Standardize Data and Business Rules
Create a standard template for each form type that identifies which fields are required, what format they should be in, and where the authoritative information lives in your systems.
Getting this right up front prevents errors down the line and stops the data entry mistakes that lead to claim denials and rework. Write down the business rules that govern each claim type (how you check eligibility, calculate coverage limits and deductibles, and decide when claims need escalation).
Step 3: Deploy Intelligent Document Processing
Configure AI and OCR to classify incoming documents and extract key fields automatically.
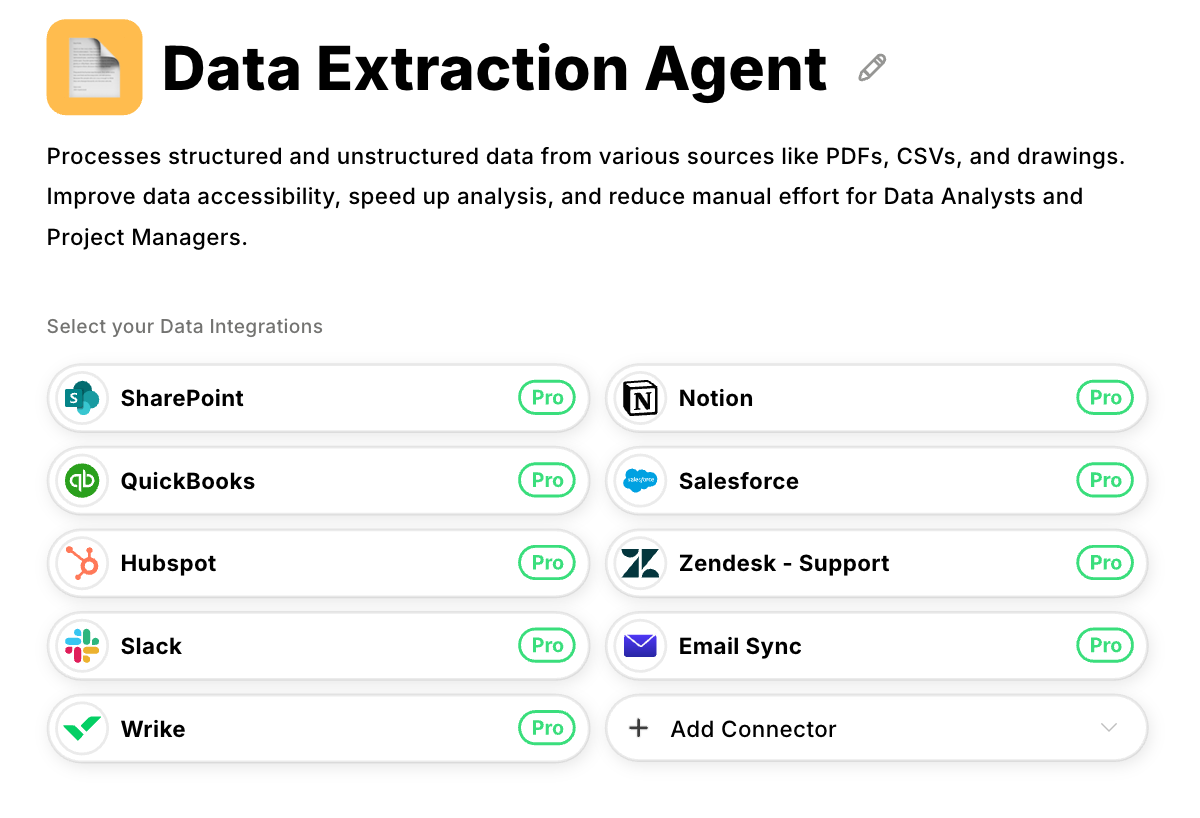
Modern extraction models routinely achieve high character-level accuracy on typed text, and Datagrid's Data Extraction Agent applies this same capability to PDFs, mobile photos, or multi-page medical charts.
Set confidence thresholds so that values above the line flow straight through, while lower-scoring fields get highlighted for quick human review.
Exceptions like missing signatures or unreadable photos route back to claimants before they clog downstream queues.
Step 4: Automate Validation and Cross-Checks
Configure the platform to compare extracted data with what's already in your core systems. Coverage status, policy limits, prior claim history, and fraud markers are all checked in milliseconds by Datagrid's Data Validator Agent.
Automating these comparisons avoids the manual costs baked into every medical claim that relies on swivel-chair lookups.
Step 5: Orchestrate Review, Adjudication, and Payment
Validation clears the way for adjudication through three processing lanes:
- Low-value, low-risk submissions meeting every rule move via straight-through processing to instant payment
- Moderate claims auto-triage to the next available adjuster with all documents pre-verified
- High-value or unusual losses route to specialists with alerts, reserves, and correspondence drafts generated automatically
Step 6: Integrate with Core Insurance Systems
Connecting your automation platform to your existing insurance systems requires technical integration.
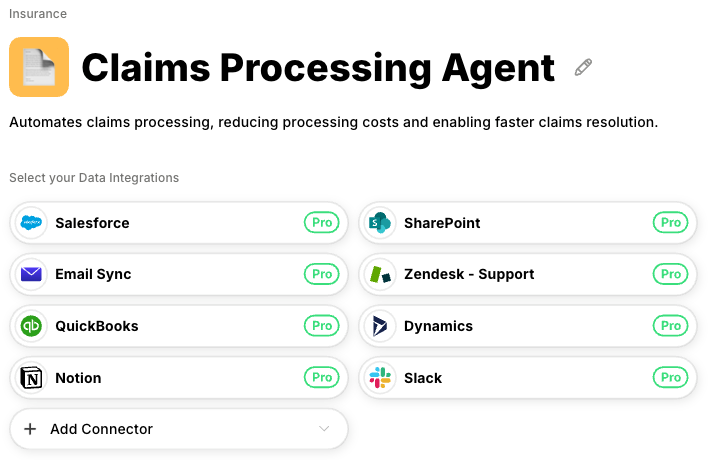
Datagrid makes this easy where the Claims Processing Agent connects to policy administration, CRM, and payment platforms so updates travel in both directions without file exports or nightly batches.
The platform includes enterprise-grade security features that control who can access sensitive claim data, encrypt policyholder information at every step, and maintain the same security standards that protect PII information.
Step 7: Measure Results and Optimize Performance
Instrument everything through dashboards that surface cycle time, error rates, cost per claim, adjuster workload, and customer satisfaction in real time.
Organizations monitoring these KPIs typically see significant cost reductions within the first year. Use the data to retrain extraction models, refine rules, and expand automation to new claim lines, turning a successful pilot into enterprise-wide transformation.
Automate Claims Forms Processing with Datagrid
Claims form processing automation eliminates the data entry bottleneck that keeps adjusters buried in paperwork instead of investigating claims. AI agents extract data from forms automatically, validate information against policy rules, and route straightforward submissions through approval workflows without manual intervention.
This transformation doesn't replace experienced professionals. It redirects their expertise toward complex investigations and customer interactions instead of data processing tasks.
Datagrid's AI agents support claims operations teams throughout the automation journey:
- Multi-format document extraction: The Data Extraction Agent processes claims forms from any intake channel, including PDFs, scanned images, mobile photos, and portal submissions, pulling structured data from medical records, repair estimates, and proof of loss statements without manual keying.
- Automated validation against policy records: The Data Validator Agent cross-references extracted claims data against policy administration systems in milliseconds, flagging coverage gaps, limit violations, and data inconsistencies before claims reach adjuster queues.
- End-to-end workflow orchestration: The Claims Processing Agent routes submissions through the appropriate processing lane automatically, from straight-through payment for low-risk claims to specialist assignment for complex losses, with audit trails generated at every step.
- Seamless integration with core systems: Datagrid connects to your claims management platform, policy administration system, and CRM through APIs that allow data to flow bidirectionally without file exports or manual handoffs.
- Enterprise security and compliance: Built-in PII protection, encryption, and access controls maintain regulatory compliance while audit trail generation supports your documentation requirements.
Create a free Datagrid account to see how AI agents can reduce claims processing time and eliminate manual data extraction from your operations workflow.